Pregnancy is meant to be a wonderful experience. However for a great deal of women the first 12 weeks or so can feel extremely unpleasant, with feelings of extreme tiredness and exhaustion to frequent bouts of nausea, not to mention the emotional reactions. For many, these feelings soon settle down and the pleasure and excitement of the pregnancy begins. But for some, the side effects of fluctuating hormones can continue and be pretty disruptive.
Pregnancy is meant to be a wonderful experience. However for a great deal of women the first 12 weeks or so can feel extremely unpleasant, with feelings of extreme tiredness and exhaustion to frequent bouts of nausea, not to mention the emotional reactions. For many, these feelings soon settle down and the pleasure and excitement of the pregnancy begins. But for some, the side effects of fluctuating hormones can continue and be pretty disruptive.
Can I have treatment?
There are situations when you may want treatment prior to your 12 week scan, to help ease morning sickness for example but generally most clients opt for treatments after the first 12 weeks have passed*. Reflexology in particular is a favourite of both ‘mums to be’ and midwives alike. As it is such a relaxing treatment it seems to never fail to bring relief from the natural aches and physical discomforts that pregnancy brings. Treatment also helps to settle and balance the hormones and most clients report great feedback from each treatment.
The Benefits
Reflexology may bring relief from the following:
- morning sickness, nausea and headaches
- swollen ankles, hands and legs, particularly 3rd trimester
- back and joint aches
- stress and anxiety
- relaxation
- digestive issues & constipation
Over Due!
In the last remaining weeks and days, Reflexology is said to be great at encouraging the body to commence delivery closer to term and support a natural labour and birth. Many of my clients have been delighted to have treatment to help relax them and ease some of the anxiety and worries that can build at this time.
Post-Natal Treatment
Once you are home and coming to terms with your new arrival, your body will be adjusting too – in an hormonal way!.. Treatment around this time is wonderful at helping the body relax again, bring about a state of homeostatis (balance) and encourage the hormones to settle – plus it’s a lovely treat after all that hard work and helps to stave off the signs of post-natal depression.
*assuming that there are no complications with the pregnancy....]]>

How Stress Can Impact Fertility In More Ways Than One!
Stress affects our overall health and wellbeing and this is no exception with infertility. Why do couples fail to conceive when there is no known medical cause?
NICE Fertility Report (February 2013) advises GPs to inform potential infertile couples of the following – 80% of couples conceive in their first year of trying naturally (women under 40 years). Of the remaining 20%, 10% go on to conceive within a total of two years of trying – therefore 90% of couples (woman under 40 years) conceive within two years of trying. With Assisted Reproductive Techniques, (ART) 50% of couples (women under 40 years) conceive within 6 cycles of IUI. A further 25% conceive with another 6 cycles of IUI.
These statistics are clearly designed to give hope to couples, however HFEA Fertility Facts & Figures Report (2008) states that 1 in 7 couples experience infertility which is approximately 3.5 million people in the UK.
Stress, in its many forms, wreaks havoc with our hormonal and nervous systems and certainly impacts upon fertility. Here are the 5 main causes of stress in fertility but don’t forget, they overlap, interrelate and are virtually impossible to separate.
Age Factor And The Pressures of Time
Infertility is the most common reason women age 20-45 seek advice from their GPs. (HFEA Fertility Facts & Figures 2008). Fertility declines with age in woman and more recently shown to be declining in men too. Draft NICE Report on Fertility (October 2012), states fertility declines with age in both women, and to a ‘lesser extent’ men.
The proportion of women having their first baby at, or after age 30 has steadily increased since the mid-70s. The probability factor for potential fertility issues increases from the age of 30 onwards (HFEA. Register Data 1991-2006 Report 2008). If couples only start their fertility journey at this age or later, then there is already a potential issue.
Not only that but the NHS will reduce the ART funding available to women aged 40 – 42 and stop funding to women over the age of 42, NICE Report on Fertility (February 2013), which will therefore affect couples that are unable to finance their own treatment.
As couples start to experience problems, they feel the pressure of the time factor and the need to try to conceive as quickly as possible to avoid either missing out on funded treatment and/or to ensure that they do not further complicate the issue as age impacts on their fertility.
Physical Stress
Physical stress can affect a couple in many ways. A significant decrease in sperm quality has been reported in research (Carlson 1992; Sharp & Skakkebaek 1993; Irvine 1996). Male factor as a percentage of infertility has increased from approximately 27.5% in 2000 to 32.5% in 2006 (HFEA data 1991-2006, extract 2008).
Other lifestyle factors affect fertility such as alcohol, coffee, weight, smoking, recreational drugs, some prescription drugs, exercise, nutrition, heat. Couples try to improve their lifestyles by abstaining from behaviours but then often feel the pressure of ‘not being able to enjoy themselves’ or turn to these behaviours when failure or disappointment occurs, adding more guilt and stress.
Many feel that after a prolonged period of ‘trying to conceive’ sex becomes ‘on-demand’, routine and pressurised, resulting in further stress to the relationship. Women particularly feel exhausted from going through a variety of tests, protocols, procedures, interventions, scans and drugs. There is also pressure from daily monitoring of their cycles or from repeated disappointment of failed treatment.
Added to which, they can experience miscarriages which prove to be physically draining and emotionally devastating. There then follows a waiting period before the body recovers and is able to start the whole process again causing more delay and more time pressures.
Emotional Stress
The pressure starts quite soon after couples begin to try for a baby. Healthy couples naturally assume that their fertility journey will be relatively straight forward. However after just a few months, doubt and concern start to creep in, resulting in visits the to GP, a string of tests and finally being diagnosed with either ‘unexplained fertility or a medical diagnosis’. This often results in a search for further assistance which can be overwhelming, time consuming and exhaustive. So, by the time the couple realise that there is a problem, they have been trying for some time. If they are not successful, the time factor increases and most if not all the stressors mentioned here start to play a part.
Physically the body is now struggling to perform or behave and the emotional stress is evident in many forms. Women particularly experience a feeling of failure and often begin to dislike their reproductive body. Depression can affect both parties. Sadness, constant disappointment and total grief are most familiar to these couples.
Some begin to withdraw from their social network as they are unable to explain their emotional state. Some suffer anxiety on may levels. Some turn to coping behaviours or such as drinking, eating etc to cope with their situation – knowing that these will only impact further on their infertile state.
Some may have subconscious blocks or fears about being a good parent or from their own childhood experiences. However, if they didn’t have any fears at the beginning of this process, they often develop them as the failure builds.
Miscarriage causes terrible emotional stress. Fear then builds as they wish to try again but are worried they will experience the same outcome all over again.
One constant pressure for many women is the inability to share their infertility problems with friends, families and employers. The process is simply to raw and they feel too vulnerable, or they fear for their careers – something that they want to keep constant in case the do not become parents. Often they have to lie about their fertility appointments – all adding to the pressure.
In his forward for Dr Sammy Lee’s, Counselling in Male Infertility, Rex Cowen wrote ‘Dr Lee points out Male patients often develop serious depression and sexual impotence following diagnosis of infertility. Once seen only as a woman’s problem, it is now clear from research that, in around 50% of all cases, a male factor is involved. Health Care professionals need to address this development and increase their knowledge and understanding of men’s feeling in coping with this difficult situation’. He goes on to describe male infertility as one of society’s taboo subjects.
Financial Stress
After trying for some time, couples often require medical intervention in the form of IVF/ICSI. Whilst they may be eligible for NHS funding initially, this funding soon runs out. Also they may want various additional tests and/or to try forms of complementary treatment. The cost of acupuncture, nutrition, hypnotherapy, reflexology, homeopathy etc can add financial pressure when in addition to private medical procedures. Multiple courses of ART, together with additional costs of donor eggs/sperm or treatment abroad can be phenomenally expensive and cause great pressure on the couple both jointly or can form a pressure between them. If they’ve had to take time off work, they may also fear for their job security too!
Relationship Stress
The pressures of trying to conceive affect relationships emotionally, sexually and financially. Throughout their entire infertility journey, they make sacrifices and changes to their lifestyles and this can lead to relationship stress. There may be disagreement about their course of action, the reason for infertility may be specific to one of them causing feelings of guilt and inadequacy, it may be the stressful stretch on finances or the lack of lifestyle ‘freedom’ that finally leads to a difficult decision of when to continue, and when to stop, or when to look at alternatives such as surrogates or adoption.
These pressures were unlikely to be present initially but build over time – most couples are unaware that they are going to experience problems with fertility and have therefore never discussed what they feel about the subject before they are already some way into the issue itself.
Many couples experience some, or all of the above pressures, which compound and may potentially account for the continuing failure to conceive despite subsequent treatment/intervention in the form of drug protocols and ART and procedures. The overall chance of a live birth following IVF treatment falls as the number of unsuccessful cycles increases. (Draft NICE Report on Fertility October 2012).
At this point they begin to feel they have run out of options – the final stress in itself. All the time there are options then there is hope, but when they have exhausted everything, they finally have to face a decision to give up, or to adopt. The adoption process in the UK is exhaustive and lengthy and not one to be considered lightly when you are already shattered from your emotional and physical roller-coaster.
Sjanie Hugo comments in her book ‘The Fertile Body Method’ (2009) ‘The role of the mind and the emotions in fertility is a vital one that is often overlooked. ‘A truly integrated approach is far more likely to give people the best possible chance of having children. Mind-body medicine is an approach to health that recognises the effect that our mind has on our body and vice versa’ …….
…….and that is why many do consider natural therapy and Hypnotherapy to help reduce the impact of Stress!!
If any of the above resonates with you and you would like to consider natural therapy such as Reflexology or Hypnotherapy to help alleviate fears, anxieties or clear emotional blocks, please do view the therapies or contact me if you’d like to make an appointment.
]]>
Are you getting a good nights sleep?
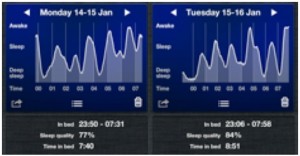
As you’ll recall I decided to use an app called ‘Sleep Cycle’ to help me monitor my sleep over a 21 day period. Throughout the 3 weeks I was to try different techniques and tips to see if I could improve my sleep. So, what were my findings?
Firstly the exercise proved to me that my quality of my sleep varies and is, at best, reasonable – not good or great. This is what I believed and the 21 day test proved this to be the case.
Ideally what I was hoping to achieve is a good night of great sleep! The app cannot measure your sleep quality but simply your movement throughout the night and this it does really well. My sleep graphs were really interesting and reflected each night as I remember it. However the app scored the quality of sleep and apparently I frequently hit 90% and above but this is definitely not my perception of the night! Over the 21 days I scored 2 nights as good (84% – 94%), 12 nights as okay (between 63% – 96%) and 7 nights as poor (47%- 98%)…. So you see my perception was, and still is, that I have, on the whole, an okay nights sleep or rest on average. Here are 3 examples of the ‘sleep cycle’ charts, 1 for a good night, 1 for a so-so night, and the chart for my worst night!:
So, what about the results for the behaviour changes etc. Week 1 was the control week where I did not change my behaviour, Week 2 I started to use certain sleep tips such as bed earlier than usual, no alcohol before bed, no caffeine, no tv in bed, read before bed, bath before bed etc and Week 3 I added exercise in the daytime and listened to a relaxing hypnotherapy cd before bed….
Did this mean that I experienced greatly I proved sleep? Well not exactly and I believe that the reason why is down to what I call ‘head chatter’. This is neither good nor bad but it is pretty common for me and consists of things running through my mind. They can be about my day, or about future concerns or ideas, they can be exciting or worrying…
Did the techniques mentioned above help with this? In parts yes… However the biggest change I noticed was from abstaining form caffeine. I did this during Week 2 and I must say that I really noticed an improved feeling of calmness, which makes sense… I only have 2 coffees a day, both before midday – to avoid caffeine in the system later in the day – caffeine can remain in the body for anything up to 14 hours, but it does seem to depend on the individual! Still, when I swapped to decaf, I had a sense of calmness.
I definitely felt improvement with slightly earlier nights and reading in bed, I also noticed that warm baths (including a soak in Epsom Salts) also helped…. The nights when I used relaxing hypnotherapy also sent me off to sleep before the cd had finished! (which is a great improvement) although I did wake with headphones still on but did manage to fall asleep again…. So all in all there were improvements but on the whole the quality of the nights sleep did not dramatically change. I should also add that on 2 nights I was abruptly woken by the screeching of foxes right outside my window, which was a shame as they were potentially good nights, and also some nights were disturbed by hormonal imbalance/heat but these things can happen at anytime.
So that brings me back to the head chatter…. There is no question that my sleep improves when my mind is in a good place!!… In other words I can do all these lovely things but if my mind is elsewhere worrying about other issues then they are all possibly in vain.
Time, therefore to address my worries and concerns… I have decided to adopt the follow technique – I have written down everything that currently concerns me…. You might be thinking ‘oh that’s just one or two things or you might be thinking oh god, that would take me ages…. well, I found it very interesting and not exactly what I thought it would be…. I made a list… Actually the list was harder to do then I expected… Because I really didn’t have THAT much on it…. I managed 10 things in general but only 2 are real worries right now and the 2 others are concerns – the rest remain ‘stuff’ that needs addressing but is not a huge worry. Alongside all of them I then wrote solutions…. Now here’s the thing… I managed to write something against everyone of them!! Where I could not find a direct solution I did have an action… Something I can do to help me get towards the solution!! So as I did the exercise I realised that only 2 things are of real concern to me and that there is always action you can take towards a solution…. Not only that but “nothing stays the same” meaning that I can take some actions now, if no solution is within my grasp then I can pop my list away for say 1 or 3 or 6 months and then have another look and see is other things have changed that may affect my actions/ solutions… hey presto! I have taken action. There is no doubt that when we ‘feel’ a little more in control of our concerns then we ‘worry’ less….
Here’s to a good nights sleep!!… If sleep is a problem for you, please do look at my other Sleep Blogs, Week 1 and Week 2 and try some of the suggestions. Also do try Hypnotherapy, as this can address specific sleep issues and also Reflexology is a wonderful relaxing treatment and many clients always comment how well they sleep afterwards - if only I could it effectively on myself!
]]> If you have read last weeks post, ‘Are you getting a good nights sleep’, (Week 1) you will know that I am working on restoring my ‘positive’ sleep patterns which have got somewhat misguided of late.Last week I monitored my sleep using the Sleep Cycle app. However I didn’t make any chances to my lifestyle so that I had a good weeks monitoring of my normal sleep behaviour. The results were interesting and varied i.e. each night appeared different on the monitor – see below:-
If you have read last weeks post, ‘Are you getting a good nights sleep’, (Week 1) you will know that I am working on restoring my ‘positive’ sleep patterns which have got somewhat misguided of late.Last week I monitored my sleep using the Sleep Cycle app. However I didn’t make any chances to my lifestyle so that I had a good weeks monitoring of my normal sleep behaviour. The results were interesting and varied i.e. each night appeared different on the monitor – see below:-
The plan this week (Week 2) is to apply the common ‘better sleep’ tips that you find in most sleep literature and information. Then I can compare the two weeks and see if my sleep pattern and quality has improved. Finally in the third week I will continue to apply the tips plus some self hypnosis! Once I have all three weeks of data I will compare and post my, hopefully successful, findings!
Common ‘Better Sleep’ Tips (I’ve amended slightly to suit me):-
- Cut out coffee and caffeine (I’ve opted for decaf but no coffee at all after 12.00 midday)
- No TV in bed
- Aim to read before sleep
- Am to be in bed by 10.00 pm
- Set the same wake time for each day – I’ll aim for 7.00 am
- No alcohol as this reduces the quality of sleep
- No sugar products/fruit before bedtime as sugar, even natural, is also a stimulant.
- No drinks to be consumed too close to bed-time to avoid breaking sleep with a bathroom visit.
- Ensure bedroom is darkened
- Ensure bedroom temperature is comfortable (not too hot/cold)
- No night-time visitors (my cat!) as they often wake and disturb
Now my rules are set, we’ll see if my sleep cycles change at all! If you are monitoring too, do make some changes from the list above and see what happens. If you need general more information there is quite a good ‘How to sleep better’ guide at www.helpguide.org.
I was also interested in how sleep deprivation can affect the production and regulations of our hormones and I was not surprised by what I discovered. Recent research by Cauter et al (2010) has the answer. They found that sleep loss can reduce the capacity to perform basic metabolic functions such as regulating hormone secretion, and in the long term could speed up the ageing process and hasten the potential onset of age-related ailments such as diabetes, hypertension, obesity and memory loss. They reported that cutting back on sleep is an extremely common response to the time pressures of modern societies. The average night’s sleep decreased from about nine hours in 1910 to about 7.5 hours in 1975, a trend that continues. Millions of shift workers average less than five hours per work day.
Their research focused on the physiologic effects of sleep loss, how sleep deprivation altered basic bodily functions such regulating blood-sugar levels, storing away energy from food and the production of various hormones.
When tested during the height of their sleep debt, subjects took 40 percent longer than normal to regulate their blood sugar levels following a high-carbohydrate meal. Their ability to secrete insulin and to respond to insulin both decreased by about 30 percent.
Sleep deprivation also altered the production and action of other hormones, dampening the secretion of thyroid stimulating hormone and increasing blood levels of cortisol, especially during the afternoon and evening.
So, it makes good healthy sense to ‘get some sleep’!
Night night…
]]> Now for those of you who know me well, will know that I am not known to be a good sleeper. In fact, I would describe myself as a ‘light sleeper’ – that is – going to bed, resting but rarely feeling that I ‘fall’ asleep – in fact the number of ‘real’ nights sleep is fairly rare for me. Last year I did wonder if I had Insomnia?! One definition is ‘habitual sleeplessness; inability to sleep’ – that kindof fits me…. but I assumed Insomniac’s were ‘up all night’ pacing, eating, reading or watching tv and just couldn’t sleep or rest?
Now for those of you who know me well, will know that I am not known to be a good sleeper. In fact, I would describe myself as a ‘light sleeper’ – that is – going to bed, resting but rarely feeling that I ‘fall’ asleep – in fact the number of ‘real’ nights sleep is fairly rare for me. Last year I did wonder if I had Insomnia?! One definition is ‘habitual sleeplessness; inability to sleep’ – that kindof fits me…. but I assumed Insomniac’s were ‘up all night’ pacing, eating, reading or watching tv and just couldn’t sleep or rest?
Wikipedia’s version is “Insomnia, or sleeplessness, is a sleep disorder in which there is an inability to fall asleep or to stay asleep as long as desired” - well, that seems to fit too – however I must say that the full definitions for Insomnia are much more complex.
Why am I interested in the quality of (or lack of) my sleep you might ask. Well simply put, sleep is of course the time when the body replenishes its energy – I would say, on all levels, physical, emotional, mental and even perhaps spiritual – for rest is extremely important to well-being.
Getting enough quality sleep and the timing of that sleep is also important. In Dr Christiane Northrup’s Women’s Bodies, Women’s Wisdom, she points out that “getting quality sleep prior to midnight appears to be more restorative to your adrenal glands (those that produce adrenalin and cortisol the stress hormones) than sleep that begins later in the night – even if you sleep late the next morning! Alcohol impacts too, two drinks per evening can wipe out your rapid eye movement (REM) sleep which is the sleep associated with dreaming – and she adds, why would you want to do this?”.
If we do not engage in the best quality of sleep and replenishment then we will encounter a level of stress, (probably subtle or mild initially), but longer periods of poor sleep will mean that the mind and body are not as alert as they could be and therefore any decisions, actions, ideas, plans, activities will be hampered by this stress. I therefore felt it was time to understand my ‘light night-time status’ and conquer the problem.
Last year I did record my sleep to ascertain if I was really having difficulty. I labelled each night as either poor (felt like I was permanently awake), okay (rested but still aware of the nights movements) or good (definitely fell into sleep at some point). On the rare occasion I did record excellent (I actually have no idea what happened during the night and woke refreshed – result!!). My findings were interesting and varied. My sleep did improve for a while but gradually became disrupted again.
So with a fresh start to 2013 I have decided to have another go. I have been introduced to a great app - Sleep Cycle* - it records your sleep pattern for the duration of the night, number of hours in bed, and calibrates whether it thinks you slept well or not?! – see the graphic below.
My plan is to monitor my sleep using this app* and to make changes, and therefore see what affect they have. I am going to record this weeks sleep (week 1) as a normal week – a control week if you like, without making any changes. Next week (week 2) I will incorporate all the usual sleep tips and recommendations such as going to bed at a set time, reading before bed, ensuring the bedroom is dark, not drinking stimulants before bed or eating too late etc and then will compare notes. The following week (week 3) I intend to use Hypnotherapy as I suspect from the early part of last year, this had a significant affect on some of my improved nights. I can then compare the weeks and see what I find! I will, of course, keep you posted each week about my findings and hopefully my improvements!
For interest, this is what my first night of monitoring looks like!!
What is your sleep like? Do you sleep really well? Or like a great number of my clients (and me), is your nights sleep broken, varied or disturbed?!
Why not join in with me and monitor your sleep cycles too! If you have a smart phone, why not download an app to monitor your sleep cycle or simply not any changes in your diary.
* One issue I do have with the ‘app style’ of monitoring is that you have to place your mobile phone on your mattress, reasonably close to your head – they suggest that you keep the phone charging while you do this. I’m afraid that I do have concerns about having mobile devices, or other electrical devices, close to your head/body for such a great length of time – especially on charge – as the surge of electricity may cause stress to the body and the phone may emit EMFs (electro-magnetic fields/currents). However as the ‘test’ is for a short period of time I shall give it a go but I have to say, it is not something that I would recommend for longer than a spot of monitoring!
]]>
I read an article in The Times a while ago (‘Could Scientists really stop the menopause?’ by John Naish, 14th July) which spoke about two new techniques that could apparently halt and even reverse the menopause. There are very good scientific and medical reasons for both treatments e.g. premature menopause brought on by cancer or other medical conditions, a revitalisation of the ovaries allowing for reproduction – sometimes science is truly amazing.
However I was shocked to read how these medical techniques can be potentially offered to create an extreme form of what they termed, ‘Lifestyle Surgery’ – designed to preserve fertility into the later years, and here I mean into our 50′s and to preserve a youthful appearance.
One technique which is already quite advanced is called ‘ovarian grafting’ – taking young healthy tissue from the ovaries, freezing it, and implanting it again when the ovaries need to be revived. The other technique involves multiplying healthy stem cells from the ovaries (in a laboratory) and re-implanting them as revitalised ovarian cells. Both techniques are clearly amazing and bring tremendous hope and benefit to young women who potentially can become infertile from their life saving cancer treatment, but should we really consider these invasive techniques in order to keep ourselves looking young?!
The article suggests that it is a question of ethics, suggesting that it is for society to decide! Understandably staving off some of the affects of menopause or the possibility of taking HRT treatment may be seen to be a good thing…. but the risk of damage to the ovaries, together with the associated health risks of more mature women having higher levels of oestrogen in their systems (than nature intended) and the potential for breast and womb cancer surely should make us think twice, especially when cases of breast cancer seem to be increasing?!
]]>
How healthy is your abdomen?
Is it stress free and happy, or is there tension, tightness and restriction hiding in the nether regions?!!
The other day I gave a new client an ‘Amno Fu’ treatment (abdominal massage), and it reminded me to do the same as it’s a treatment thats definitely top of my list for sorting out ‘tummy tension’ which can ultimately lead to lower back pain and bloating.
It never ceases to amaze me that a pocket of tension is lurking in my pelvic area or that I’ve tied my tummy in knots.
How does it get there and Why? Well, the answer of course is varied, and probably depends on a number of factors. As unique individuals we manifest our mental and emotional stress into our bodies, very differently.
For me, I get classic neck and shoulder tension, but with a nice dose of tummy tightness. By the time I’ve realised, I’m suffering from sciatic pangs, sleeplessness, digestive issues, not to mention the hormonal bloating that can be uncomfortably present every month.
Then there is the energetic relationship – you could ask ‘what is it that is hard to digest’ or ‘what is difficult to let go of’ and, once in tune with my tum, I am sure that I could come up with several answers for you.
Lets not forget the emotional factor – I often feel ‘lighter’ after treatment, as if I’ve managed to release some emotion that was lurking in the depths – forgotten but not forgiving.
After her treatment my new client commented ….’I really do feel incredible… such a funny / nice feeling!’
Do you suffer from lower back ache or sciatic pain?
Do you have fertility issues? Or have you previously had a pelvic or gastric operation?
Perhaps an Amno Fu treatment could help you? do have a look at my website for further details if you think it might.
]]>
I have always suffered from monthly ‘breast tenderness’ but like many women I was simply unaware that repeated breast pain or tenderness is a ‘real’ condition known medically as Mastalgia – it literally means ‘pain in the region of the breast’ and is divided into two types, Cyclical or Non-Cyclical.
Cyclical Mastalgia relates to the hormonal cycle and commonly occurs in the days prior to bleed or sometimes, around ovulation. Breasts feel heavy, swollen, tender and uncomfortable. Non-Cyclical Mastalgia is unrelated to the hormonal cycle and may affect one breast only where Cyclical Mastalgia usually affects both. Symptoms are similar but also include discomfort around the ribs.
If you suffer any discomfort that is not part of your normal monthly cycle, or are concerned about Non-Cyclical Mastalgia, you must consult your GP immediately.
Breast pain/tenderness, as part of your cycle, is often dismissed as a hormonal symptom of no real concern. However for many women, it can severely impact on their lifestyle. The discomfort can be so severe that you can’t run or exercise (I even find running upstairs painful), touch or intimacy is out of the question, sleeping on your front is impossible and usually results in wearing a bra to bed for support. Bra’s and tops don’t fit at this time and other symptoms are usually present such as feeling emotional/tearful for no reason. The discomfort lasts from a few days to up to 7 – 10 days at a time.
But this is more common than we think. According to the Maidstone Breast Clinic, between 50-70% of women suffer from breast pain at some point during their lifetime – see their website for more in-depth information.
So, what can you do about it? Firstly, it is always important to seek medical advice if you have concerns about your symptoms. Charting your discomfort frequencies and levels provides good evidence – use the Monthly Cycle Monitoring Chart to help monitor your symptoms.
Some evidence suggests that caffeine and fatty foods aggravate the condition – reducing or cutting these out of your diet may help to improve the problem but this is not always the case. Taking Evening Primrose Oil is often recommended but apparently needs to be taken for 4 months before any improvement is seen, however this does not work for everyone. Equally taking the Contraceptive Pill for some helps the problems and for others aggravates the problem. Hormone Replacement Therapy can also cause breast pain. There are some drugs that can be prescribed that may help but these of course must be discussed with your GP and are perhaps your last resort.
So it appears that this is a very individual issue, as of course, are hormones and our cycles which is perhaps why, we rarely discuss breast pain – however, there is a great deal of information available that you might find helpful rather than simply suffering every month or so. Please use the Monthly Cycle Monitoring Chart to monitor your symptoms, arrange to see your GP if you have concerns, read up on Breast Pain to become more informed. Such sites as the Maidstone Breast Clinic, Breast Cancer Care, London Breast Care Centre are all very informative.
Above all, please do not suffer in silence, ask for help, perhaps some of the advice available may alleviate your symptoms.
Do comment on this blog if you suffer such discomfort.
]]>
It strikes me, as I research this subject, that there are a great many sites and organisations devoted to this area and whom specialise in providing help and support be it onscreen, on the phone or in person¹ – The Miscarriage Association provide some really good downloadable information on their site (see below). Still despite this assistance, many tell me how emotionally and physically devastating Miscarriage and Pregnancy Loss can be. All we can do to help is to provide as much support and advice as possible.
Pregnancy Loss is very common – approximately 1 in 4 pregnancies end in miscarriage³. It can happen at any time during the entire term but is most common in the first Trimester – usually pre 10 weeks although perhaps not discovered until the 12 weeks scan.
A ‘Chemical or Biochemical’ pregnancy is one that is lost prior to confirmation by an ultrasound scan. A ‘Clinical’ pregnancy is one that is lost post confirmation by scan. Both terms are viewed as ‘medical/clinical’ and don’t appear to adequately or emotionally describe the ‘pregnancy’ that is owned by the potential parents. The new terminology of ‘Pregnancy Loss’ rather than Miscarriage is hoped to be more sensitive.
Early Pregnancy Units (EPUs) are available at most NHS Hospitals and provide emergency care, help and support for those needing assistance with a pregnancy related problem. However some units provide more care than others and opening times vary i.e. some are only open Monday to Friday, whereas others are also open on Saturdays.
Some GPs recommend trying to conceive straight after a Chemical/Biochemical pregnancy but often suggest waiting for the body to normalise after a Clinical Pregnancy Loss.
However from an emotional point of view, when dealing with your grief and loss, you are unlikely to differentiate between either of the above. Whichever way you look at it, a pregnancy is a pregnancy and a loss is a loss. Every individual/couple will deal or cope with this in a very personal manner – best advice would perhaps be to say, do what feels right for you and take your time. Ask or seek help and assistance should you feel it necessary – there are many organisations out there wanting to help….. and please, don’t forget the men – their loss is often as greatly felt but not necessarily shown, nor sometimes considered…..
Do contact The Miscarriage Association, www.miscarriageassociation.org.uk; and The Association of Early Pregnancy Units, www.earlypregnancy.org.uk for further information.
I feel strongly that the emotional and physical trauma should be treated in the very least holistically and spiritually, as the impact is often silent but felt very individually.
Despite the fact that this is sadly a very common occurrence, often little help and support is provided and very little information is given to those in need at the time. Many have shared their experiences in the hands of staff who lack any understanding or empathy in such circumstances.
As a Reflexologist and Hypnotherapist, I strongly recommend Reflexology to help the body to hormonally rebalance after such a trauma. Time and time again I have seen great benefit from such a rebalancing treatment. I also feel that Hypnotherapy can help to address the emotional stress often caused by such circumstances, which can often lay dormant for great lengths of time.
It is true to say however that a great number of women/couples who suffer from such loss, whether primary or secondary, do go on to conceive healthily.
]]>For some getting pregnant can be reasonably straight forward. For a larger number of 30 somethings, it can be a roller-coaster of cycle monitoring, tests, more tests and procedural failures, and for others, it just doesn’t happen…
You would think therefore, that when you finally fall pregnant you would be elated, and overjoyed, and swinging from the rafters?!
However, this is often just not the case. Many of you spend your entire pregnancy in a state of anxiety and worry, especially if it has taken a great deal of time and effort to achieve, your concerns often based on a previous trail of failed IVF, miscarriage, hopes and disappointments.
Here are some thoughts and feelings of one of my clients…
“After the initial elation (and disbelief) I am trying really hard not to worry constantly. I feel completely fine but I’m almost wishing morning sickness on myself so that I ‘feel’ pregnant! I’m trying to stay neutral – not get too excited, just in case, but at the same time, why shouldn’t I? We’ve been waiting for this for so long and surely if I think positively, that’s half the battle? I kind of feel in limbo at the moment….”
This lady is hoping that after her 12 week scan, her fears will die down and she will be able to enjoy the remainder of the pregnancy and I’m sure she will. But for many I know that the fears simply continue and at times even grow… and the entire term stretches out in front of you in a daunting number of weeks, broken up by the thought of the next scan date or check up.
So, what positive steps can you take to support yourself through this time?
Here are some things that my clients have found genuinely really helpful:-
- If possible book an extra scan for reassurance
- Try the Baby Heart Beat Monitor for peace of mind – can be used anytime.
- Try Hypnotherapy cd’s for relaxation or a Hypnotherapy session to help alleviate some worries
- Read helpful articles or blog posts or on-line forums
- Talk to a friend or supportive person – away from your relationship – someone who has been through a similar experience or someone who works in this field such as your Midwife, Doctor or Therapist.
- Gentle exercise is known to help relaxation – try Pregnancy Yoga and Swimming.
- Ensure you’re eating well – apparently B Vitamins found in wholegrains increase levels of serotonin (the anti-stress hormone).